It is becoming increasingly popular for women who want a low-intervention birth to opt for natural birth in hospital, because it gives access to medical support if needed.
In this article, we’ll explore some key tips for achieving a natural birth in hospital, including birth plans, finding supportive healthcare providers and hospitals, hypnobirthing techniques, natural pain relief options, positive mindset and openness to changes.
But first, let’s start with the biggest tip of all…
Table of Contents
- Avoid “The Cascade Of Interventions”
- Write a Birth Plan
- Choose Your Hospital Carefully
- Learn Hypnobirthing Techniques
- Research Other Pain Relief Options
- Stay Mobile During Labor
- Find A Supportive Birthing Partner
- Stay At Home As Long As Possible
- Prepare Strategies To Make You Feel Safe
- Consider Using Water
- Don’t Be Afraid To Ask “Why?”
- Natural Birth In Hospital Conclusion
Avoid “The Cascade Of Interventions”
Childbirth is a complex and dynamic process, and hospitals generally have protocols in place to ensure the safety of both the mother and baby.
These protocols also help avoid finger pointing if something goes wrong “on their watch”.
The tendency, therefore, is for hospitals to make interventions along the childbirth process to monitor and speed things along.
The problem, as outlined in a 2013 research paper published in the Journal of Perinatal Education, is that seemingly harmless interventions can have unintended consequences that lead to the need for more interventions later on.
This is known medically as the “Cascade of Interventions”.
Here are some of the common hospital interventions and their consequences:
Bed Rest / Reclined Position
On admission, the first well-meaning intervention given by most hospitals is to put the laboring mother to bed, reclining or lying on her back.
This can result in a longer and slower labor, contractions that are weaker and less effective, and can create difficulties for the baby descending into the birth canal.
The best thing for a laboring woman is unrestricted movement.
By allowing her to find the position that is most comfortable for her, and the ability to stand, kneel, or lean as required, means she is likely to experience less pain overall.
Free movement also increases the quality and effectiveness of her contractions, and uses gravity to help the baby move into the right position.
This becomes especially important in the second stage of labor, where the traditional “lying on your back with your knees in the air” position favored by medical staff can actually increase the amount of pain and the likelihood of needing an intervention such as vacuum or forceps, episiotomy, or even caesarian section.
Instead, it’s far better to work with gravity and “labor down” from a standing, kneeling, or squatting over a birthing ball.
Electronic Fetal Monitoring

Pretty much as soon as you are put into bed, the Electronic Fetal Monitoring (EFM) starts.
This can restrict movement further, while they get the readings they want, and may go on for a prolonged time. This, again, can lead to higher rates of vacuum or forceps deliveries, and also caesarian sections.
During the birth of my first son, I was hooked up to EFM for hours, because he was asleep and they didn’t get the readings they wanted.
This was a source of anxiety to me, which slowed the whole process down.
Limited Food and Water
Some hospitals have a policy of restricting food and water intake in case anaesthesia or a c-section is required.
This can increase the amount of stress the laboring mother feels, and causes dehydration and early exhaustion, which again slows down labor.
Unless you have a high risk pregnancy, it’s far better if you are able to eat and drink as your body needs to keep your energy and spirits up.`
Vaginal Exams
Studies have shown that excessive vaginal exams can increase the risks of infection, including neo-natal sepsis and streptococcus in the newborn. Treatment of these infections can then lead to Asthma and an increase in allergies.
One study showed that seven or more exams during labor made infection 4.5 times more likely.
Each vaginal exam also requires a prolonged period of lying back, which as we’ve discussed, reduces the frequency and effectiveness of contractions, and leads to the need for medical intervention and perhaps even c-section.
Ideally, you will have a vaginal exam on admission, to determine how far along you are, and then the perhaps a final one as you reach transition.
Induction of labor
A common intervention is to “help” the labor along with a dose of Pitocin to stimulate contractions, and perhaps prostaglandin gel to help “ripen” the cervix.
By and large, these interventions are for medical efficiency, not your benefit, and they can lead to complications and the need for more interventions later.
These interventions can create powerful contractions that require administration of pain medication, and can overstimulate the uterus, causing fetal distress and in some cases, uterine rupture and perineal tears.
This starts a cascade of other interventions, such as pain medication, fetal monitoring, repair of perineal tears, instrument assisted birth, neonatal resuscitation and even caesarian section.
Amniotomy or Membrane Sweep
The amniotic sac is there to protect your baby from infections, as well as buffer them from the intensity of contractions. In a natural birth, your waters will break as the baby moves into the birth canal ready to be born.
Some hospitals may offer to rupture the membranes to speed up the labor, but studies have shown this is of limited benefit, and can put mother and baby at increased risk of infection and complications such as prolapsed umbilical cord.
The infection risk also sets a deadline for delivery, which can lead to higher rates of c-section, instrument assisted delivery and fetal distress.
Epidural

Anaesthesia such as epidurals can slow down labor and reduce the effectiveness of contractions. As above, this can lead to higher use of instruments (vacuum or forceps), as well as caesarian section.
They also carry an infection risk to both mother and baby, such as fever and sepsis and can interfere with both lactation and the baby’s breast seeking instinct.
An epidural can also lead to bladder issues, such as urinary retention, resulting in the need for a catheter.
Catheterization
Catheterization carries a UTI infection risk, requiring antibiotics which in turn increase the risks of allergies and asthma in the newborn. They also interfere with mobility, which as discussed above, slows down labor and the quality of contractions.
Episiotomy, Instrumental Assistance and Caesarian
The use of epidural to break the pain feedback loop can cause problems pushing – it either becomes ineffectual or the mother pushes at the wrong time because they are out of touch with the sensations in their body.
Combined with limited mobility and the traditional “knees in the air” posture favored by medical staff, this can lead to the need for instrumental delivery, such as forceps or vacuum extraction, or in the worst case, a c-section.
Instrumental extraction puts the baby at risk of brain and eye problems, and nerve damage.
Vacuum extraction also carries the small but serious risk of blood pooling and clotting in the scalp, which can be life threatening.
The risks of instrumentation assisted birth (and the general cascade of interventions) can ultimately lead to caesarian section. This, despite being fairly commonplace, is a major surgical procedure, which carries its own set of risks.
Example of a Cascade of Interventions
Around 85% of U.S. women will have at least one medical intervention during birth, especially in hospital, so it pays for both you and your birthing partner to be fully informed and aware.
That way, you won’t be easily swept along into a cascade of unnecessary interventions, that are more for the benefit of the hospital than for you and your baby.
Here’s how seemingly harmless interventions can cascade:
You are admitted to a bed and lay reclined on your back while they perform initial fetal monitoring.
The position and lack of movement causes your contractions to slow down and become ineffective.
You are offered Pitocin (Oxytocin) to speed up your labor
This requires you to have more intensive fetal monitoring, further limiting your movement, and causes more painful contractions, leading you want to want an epidural
Your slow contractions and lack of feeling from the epidural lead to prolonged labor, exhaustion, ineffective pushing… until you end up needing a vacuum or forceps assisted birth.
This results in tearing down below, or the need for an episiotomy.
So where possible, you need to be cautious about accepting interventions, and be clear on whose benefit they are for.
This was something I found from first hand experience in the birth of my first son (read my birth story here).
I was convinced to lay on my back by the medical staff because it was more convenient for them to keep an eye on things, which caused my contractions to slow down and made his passage down the birth canal much harder.
My hypnobirthing book has more tips on giving birth naturally.
Write a Birth Plan
One important aspect of a natural hospital birth is having a solid birth plan that outlines your preferences and goals for the birth experience.
A birth plan is a document that communicates your wishes and preferences for your labor and delivery to your healthcare team.
This can include preferences for pain relief options, the use of medical interventions, and the overall atmosphere of the birthing room.
By communicating these preferences to the healthcare team in advance, you can feel more in control and confident in your birthing experience. It also gives your birthing partner something to refer to when advocating for you.
Be aware that most nurses won’t have time to read pages and pages of notes, and may take your wishes less seriously if your birth plan looks like a celebrity rider.
So try and keep your birth plan to a single page. We cover birth plans in more detail in our hypnobirthing book.
Choose Your Hospital Carefully
Not all hospitals and healthcare providers are created equal when it comes to both natural births and birthing techniques.
So it’s important to research and interview potential providers and hospitals to find ones that are open to your preferences and have a supportive and empowering approach to childbirth.
There are generally three types of setting where you can enjoy natural childbirth with medical support.
The first is a dedicated birthing center. These are generally run by trained and experienced midwives who can handle most situations, but they do not have immediate access to OB/GYN surgeons or advanced medical interventions in house.
The second is a birthing center attached to a hospital. These, again, are usually midwife led, but with the advantage of being in or near a hospital with all its life saving technology.
The third is the maternity ward of a regular hospital. These tend to be doctor-led with midwife and nurse support.
Usually, the best of both worlds is the second option – a dedicated birth center attached to a hospital – because they will likely not be as rigid in their protocols as a hospital maternity ward, and you can usually avoid unnecessary medical interventions while having the reassurance that instant access to life saving technology is available should it be required.
I gave birth to both my sons in the hospital. The birth of my first baby was in a more traditional hospital setting (though we had a private room), and it was hard to avoid unnecessary medical interventions.
The second was at the same hospital, but being 18 months later on, they had added a midwife led maternity unit which was much more flexible to our wishes.
Learn Hypnobirthing Techniques

Hypnobirthing techniques can also be useful in achieving a natural birth in the hospital.
Hypnobirthing involves using self-hypnosis, visualization, and relaxation techniques to manage pain and stay calm during labor. This can speed up labor and avoid the need for epidural or other pain relief.
Hypnobirthing can be taught through classes or self-study, and can help you feel more in control and relaxed during the birthing process.
You can download my hypnobirthing book and MP3s and get started right away!
Research Other Pain Relief Options
Pain relief options are another consideration for natural birth in the hospital.
While the goal is to avoid medical interventions and pain medicaton, it’s also important to recognize that labor can be physically and emotionally challenging.
There are many natural pain relief options available even in hospital, such as massage, hydrotherapy, and aromatherapy, and these can be coupled with hypnobirthing techniques like visualization, affirmations, and meditation to manage pain and stay relaxed during labor.
You can also have low intervention pain relief, such as gas and air, which can help give some respite if things become overwhelming.
See our article on Pain Management During Labor for more information.
Stay Mobile During Labor
Standing, squatting, rocking, walking… it doesn’t really matter how you move, as long as you keep moving during active labor.
Movement reduces tension and helps work with gravity to allow your baby’s head to move into the correct position for birth. It also acts to distract you from discomfort and gives you something to occupy your mind.
When I explained the importance of this to one expectant mother, she said, “oh, it’s like jiggling the cork out of a champagne bottle”.
And that really sums it up well. Movement just helps your baby find their way out!
Find A Supportive Birthing Partner

Maintaining a positive mindset and supportive environment is also crucial for a successful and satisfying hospital birth. Fear and anxiety can increase pain and stress during labor, so it’s important to stay calm and centered.
Creating a positive and supportive birthing environment, with calming music, dim lighting, and familiar objects or scents can help, but knowing you have the support of your birth partner is often the most important consideration.
When we are scared, in pain, or feeling helpless, it’s easy to have your mind swayed by an authority figure, such as a doctor, nurse or midwife.
That’s where birth partners are super valuable.
This was something I learned first hand during the birth of my first son. My husband, Rob, had gone to get the bags and within the space of 10 minutes, I’d been convinced to give birth on my back. He came back and was confused by my apparent change of mind.
So you need to be clear before you start on what you want, so your birth partner can properly advocate for you if you need it.
And if you don’t have someone to act as your birth partner (spouse, parent, friend etc) then consider hiring a professional doula.
Stay At Home As Long As Possible
Most women find home the most relaxing and comfortable place to be. You have all your familiar things around you, and it feels like a safe space to get into the rhythm of labor.
You can move around freely, find things to distract yourself. Many mothers (myself included!) find themselves with the urge to “nest” by cleaning and vacuuming the house, and this natural movement also helps to speed up labor.
You can also eat and drink as you wish, take time to rest or be active, and consciously prepare yourself for the birth experience.
More importantly, you can avoid unnecessary medical interventions such as constant fetal monitoring by staying at home until you feel the time is near.
I’m not advocating home birth. It’s much safer overall to give birth in the hospital, but the minute you arrive at hospital, you’re telling them you expect to give birth soon – and hospitals specialize in interventions to make that happen faster!
So unless you have been able to find a midwife-led birth center that has a looser protocol to the hospital maternity ward, or have a high risk pregnancy, it’s usually best to stay in control by staying away from hospital until you really feel ready to go in.
Prepare Strategies To Make You Feel Safe
Fear is the contraction killer that can stop labor in its tracks.
It makes sense if you think about it. After all, it would make no sense to go deliver a baby into a dangerous environment. So when you feel fear, the body tries to delay delivery until you are away from danger.
The problem is, it can’t tell the difference between real physical danger, and the fear and anxiety caused by being a helpless medical plaything in the bright lights of the hospital.
So before you go to the hospital, think about things that make you feel safe and secure, and how you can bring those safe feelings with you to the hospital.
Familiar clothes, dim lighting, soft music, familiar smells can all help create a safe space that helps your contractions strengthen and move labor forward.
My hypnobirthing book covers some more strategies for keeping that feeling of being calm, relaxed and in-control.
Consider Using Water
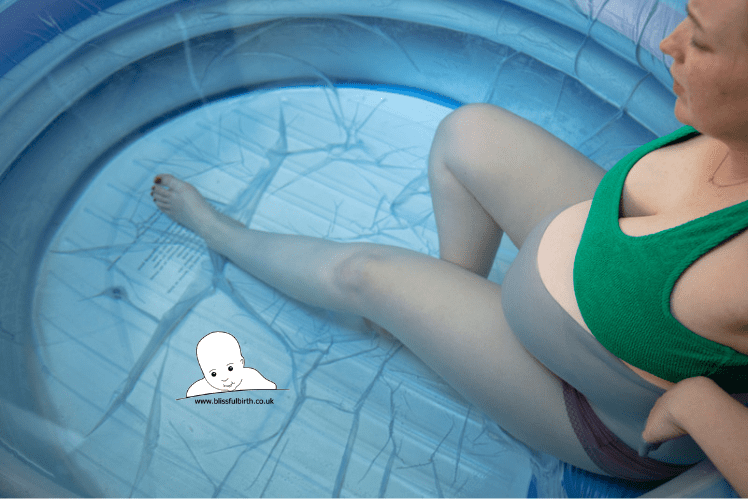
Even if you are not having a water birth in hospital, you may still wish to use water to help release tension and ease aches and pains.
Many birth centers have showers or tubs you can use to distract yourself and make yourself feel more relaxed. Or you might just want a cooling towel on your forehead.
Many expectant mothers love nothing more than the feeling of warm, soothing water on their skin, and it can be just what you need to feel re-energized during labor.
Don’t Be Afraid To Ask “Why?”
Remember that you have the right to make informed decisions about your birth experience.
Remember also that giving birth in a hospital, surrounded by experts in uniforms, can make you feeling more vulnerable and open to their agenda and suggestions than you might otherwise be.
So if you feel that your wishes are not being respected or that you are being pressured into interventions, don’t be afraid to speak up and advocate for yourself.
Part of feeling in-control during birth in a hospital is asking questions before consenting to an intervention. Remember that, once started, even simple interventions can be a slippery slope to more serious ones.
Some questions I found useful to ask when an intervention was being offered, were: “Why is this needed?” and “How does it benefit me and my baby?”.
You can also ask, “What are the risks to me and my baby if I say no?”
This is also where a supportive birth partner can be your rock by advocating on your behalf to ensure any interventions are wholly necessary and not just a convenience or liability covering exercise for the hospital staff.
Natural Birth In Hospital Conclusion
If your goal is a natural, unmedicated birth, with the support of medical intervention if it is required, then a hospital birth generally provides the best of both worlds.
With these tips, you can have a safe and satisfying hospital birth with minimal medical intervention.
That said, it’s important to remember that every birthing experience is unique, and there is no one “right” way to give birth.
And for hospital staff, there is a fine balance between prioritizing the health and safety of the mother and baby, and honoring the mother’s preferences and goals.
Their ultimate goal is a safe delivery and a healthy baby, but they are human beings and will tend to choose what is convenient and familiar for them if you allow it.
Finding a birth center that is flexible and supportive, as well as being personally flexible to unexpected circumstances that could change your plans, will allow you to enjoy a natural hospital birth that is aligned with your goals for natural birth.
Do you have any more tips for a natural hospital birth?
Did you find a natural birth friendly hospital? Was a hospital birth the best of both worlds for you? Share your inspiring stories below!